Core Facilities
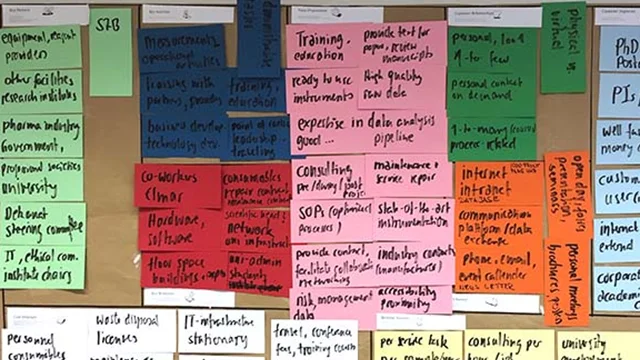
Every Researcher in experimental science should have access to state of the art technologies, independent of the size of his lab or his affiliation with an Institute. Thats the basic idea behind Core Facilites. Core Facilities are the place to share high prized instrumentation and sophisticated methods, accompanied by the expert knowledge of their staff to use them in the most efficient way. And they should have a time saving organisational framework to find and access the Core Facilities and to design your experiments and daily research life.

Booking System
PPMS is a web-based, booking and management software system for the operation of core facilities, shared resources and technology plattforms. We are currently implementing the system across the University of Bonn. The software itself offers a one stop shop solution, providing researchers an easy way to access cutting edge technology.
Registration
We will need your contact data and a cost center to grant you access to our PPMS Booking system.
640+
registered users
25+
Major Instrumentation
24.000 h/a
Booked Measurements
Your Acknowledgement Matters!
And it is more than a nice way to say "Thank you"
Or more official: ... publications must contain a reference to the DFG funding (so-called "Funding Acknowledgement") in the following form: "funded by the Deutsche Forschungsgemeinschaft (DFG, German Research Founda-tion) – project number(s)"...
Find more information following the LINK below.

Because it makes sense, both scientifically and economically. Core facilities do not only provide technologies and services, but are run by experts to assist with your research. You are collaborating with professionals who specialize in helping you obtain, analyse, and interpret high quality research data. And they have the time and mind set to do so. Moreover they help you to avoid errors from the beginning and reduce the time to get people on the job. So unless you have the resources to hire a full-time, PhD-level specialist to maintain expensive instrumentation and provide sophisticated services, it makes sense to look at the core facilities we offer.
You are nearly there. We created similar web pages for each core facility, that should provide the information for a first contact. So take a look at the collection of core facilities and then simply call, email or stop by the core facility that you want to work with. And keep in mind that our supportive staff is occasionally very busy, but will find some time to discuss your research needs with you. Core facilities that use online booking and submission will guide you through the onboarding process to the Stratocore PPMS booking system.
Most of the measuremnt time on our instruments is managed by our PPMS Booking and Managment System. We are in the process of migrating it to a shibboleth authentication. But for the moment you register using this LINK and once you are introduced to the system and trained for the machine, you can make a reservation, run your experiment. For more details see the getting started section on the webpage of the corresponding core facility.
Definitly! Our core staff are experts in various research areas and can accompany you on your journey from the idea to the publication. To get an impression see the News Archive and try the Search Engine.
Feel yourself invited ! Many students use our cores and we are happy to train the next generation of scientists. Remember that not a few professors and prize winners started as students using our core facilities here in Bonn. But you have to keep in mind, that only the basic introduction into the technology and education is free of charge. In general the costs of the services in the core facilites are at the users expense. Whereas talking is for free.
We selected and applied for instrumentation, that can be used in an autonomous fashion. Some cores offer trainings for using this type of instrumentation. Please reach out to the core you want to work with, and they can help you schedule training.
User fees are unique to each core and are posted on their individual web pages. Our user fee structure is designed to comply to Funding Guidelines of different funding agencies and the DFG guidance for core facility usage costs (DFG form 55.04 – 07/24). For internal users we will only charge project specific costs. That means we will not make profit from internal users, nor are we allowed to charge users for any expenses already covered by grants or other funds. In general, user fees represent the overall consumables and staff costs of a particular service, not including costs for basic operation, repair and maintainance. Thanks to ongoing subsidy support from the faculties and the university, cores can offer services to an attractive price relative to the true market value of those services.
Sorry to say, but this does not account for external academic or industrial partners. Nevertheless the core staff can help you estimate project costs as needed and find the appropiate person to deal with contracts or cooperative research projects.
As is mentioned in the DFG form 52.01 – 09/24 Basic Module under 2.5: "Funding may also be requested for user fees for major instrumentation and core research facilities. The DFG can only cover such costs that are required specifically for the project."
We would recommend to ask the core facility for a cover letter, where the core facility states, that the needed technologies and capacities are present and that the costs are calculated on the basis of project specific additional costs as described in DFG form 55.04. "Funding for core facility costs in Collaborative Research Centers", in EU or BMBF projects might require some more consultation to use the correct wording and placement of costs within the application. The "Research and Innovation Services" of the university are always willing to help you on that topic.
Yes please! Acknowledgements are one of our most important metrics for research impact.
And remember the DFG Code of Conduct. "Authorship is justified for an individual who has made a genuine, identifiable contribution to the content of a research publication of text, data or software ... If a contribution is not sufficient to justify authorship, the individual’s support may be properly acknowledged in footnotes, a foreword or an ac- knowledgement.
Moreover for usage of DFG funded instrumentation, you have to acknowledge the core facility. Find more information HERE
Contact
Elmar Endl
Alte Sternwarte
Poppelsdorfer Allee 47
53115 Bonn